Osun’s Overburdened PHCs Struggle to Deliver Essential Patient Services Due to Staffing and Equipment Shortages.
Uche Oti
12 min read . Jul 9, 2024
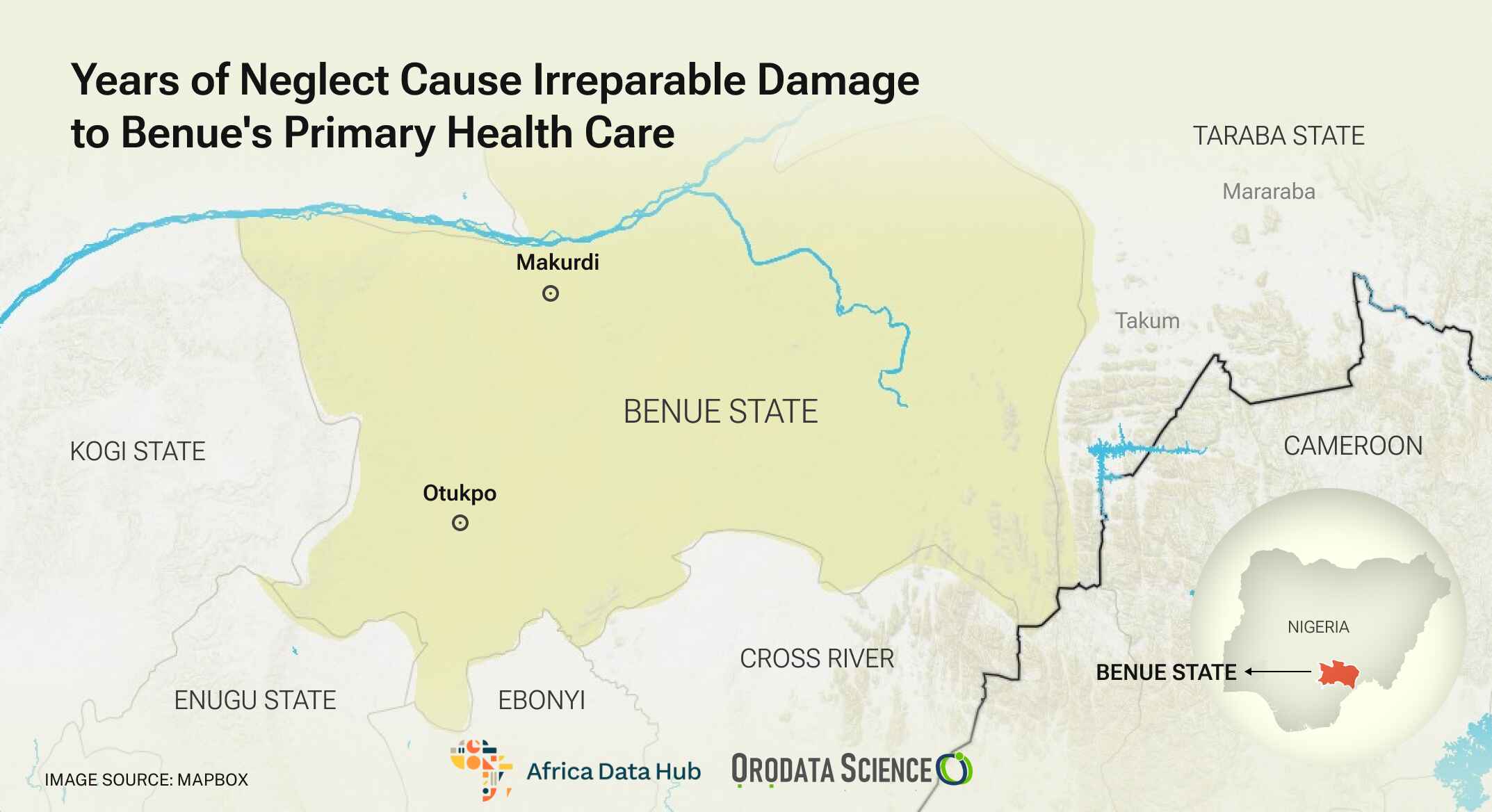
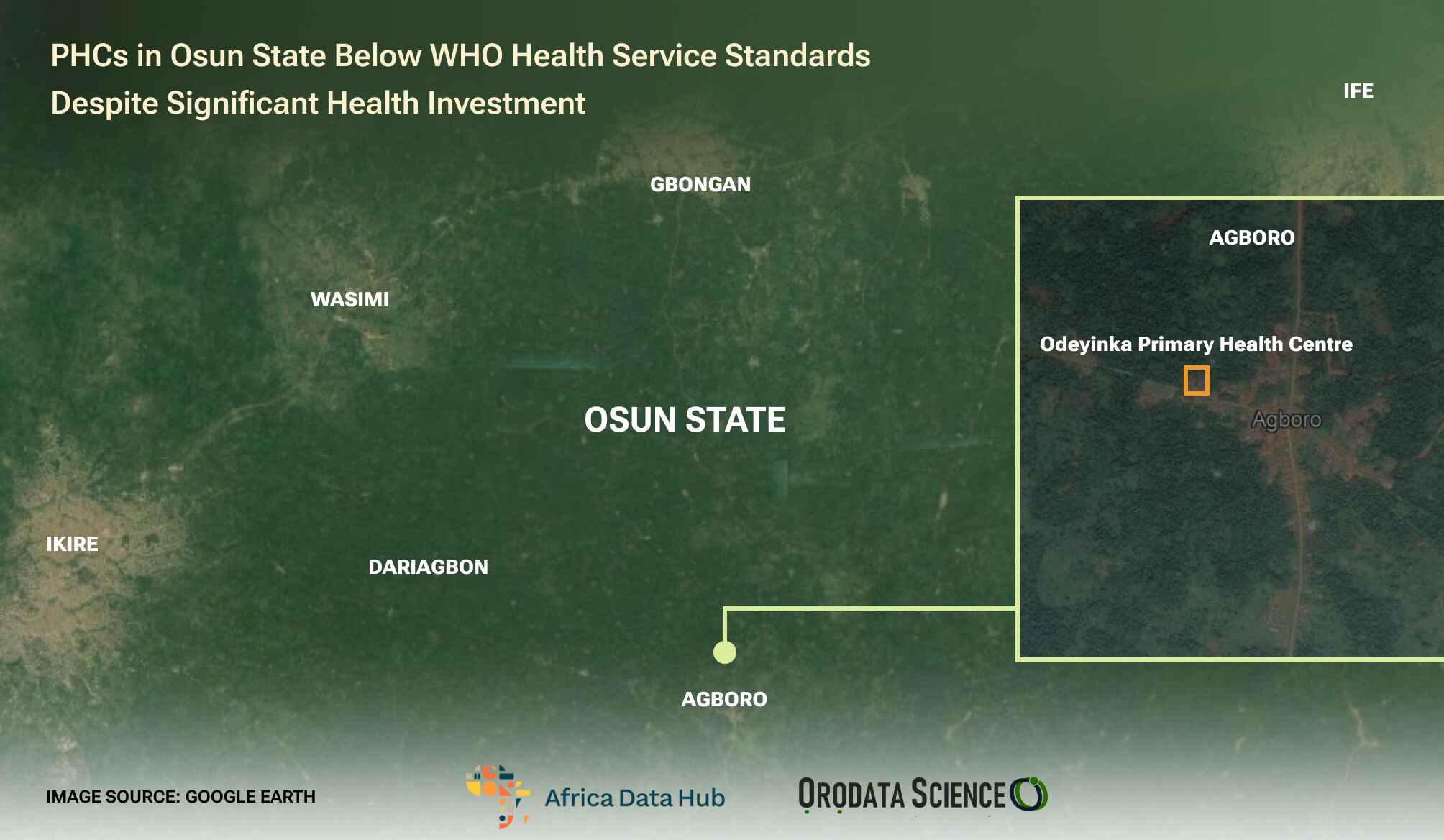
In 2022, a heart-wrenching incident occurred in Odeyinka, a small community in Ikire, the headquarters of Irewole Local Government Area of Osun State in south-west Nigeria.
A pregnant woman, Bidemi, was admitted to the Odeyinka Community Health Centre, a primary healthcare centre (PHC). That same day, she delivered a baby boy, but because the centre lacked adequate medical facilities to manage the excessive blood loss she experienced during childbirth, she was referred to another hospital in Ikire town. Still, the family was dissatisfied with the handling of her case in this second hospital.
Her husband decided to take her to their hometown, Cotonou in Benin Republic, for further medical attention. But the woman unfortunately died on their way to Cotonou a week after her delivery. Three days after the woman’s death, her son also died.
Eunice Ogundele, the only health worker in the PHC in Odeyinka, said the report she got indicated that the woman lost a lot of blood and never got well until she died.
She also said the baby became ill and did not recover.
“I was told that the child began to show very serious signs of illness. They took the baby to the hospital but I guess it was too late. The woman’s husband came back to pack their things and left for Cotonou after the child died,” Mrs Ogundele, a health technician, told PREMIUM TIMES.
The health technician, who took the delivery of Bidemi’s baby, described her situation as sad.
Nigerians need credible journalism. Help us report it.
PREMIUM TIMES delivers fact-based journalism for Nigerians, by Nigerians — and our community of supporters, the readers who donate, make our work possible. Help us bring you and millions of others in-depth, meticulously researched news and information.
It’s essential to acknowledge that news production incurs expenses, and we take pride in never placing our stories behind a prohibitive paywall.
Will you support our newsroom with a modest donation to help maintain our commitment to free, accessible news?YES, I’LL DONATE TODAYxDo this later
However, two years after the tragic incident shook the small community, it is still fresh in the minds of Mrs Ogundele and others who know the family of the deceased. Many residents of the community believe the death could have been averted.
Apart from having only one worker, the Odeyinka PHC is insufficiently equipped.
“The PHC lacked both the necessary staff and medical supplies to address the woman’s condition,” Mrs Ogundele said, stressing that the deceased and her baby would not have gone through their harrowing experience if the centre had adequate support.
She recounted that she asked the woman to go to another hospital because she needed more extensive medical attention after the delivery.
Dilapidated facility
When this reporter visited the facility in October 2023, it was under lock and key and the door was covered with a mosquito net. Inside the facility, this reporter discovered that there were no beds, bandages, gloves, syringes or other vital items needed for treating or attending to patients.
Virtually everything in the centre was old, damaged or dilapidated. The building’s perimeter fence and entrance door were an eyesore.
There was also a bowl used to collect rainwater from the roof, and a dirty well, which are the only sources of water for this PHC.

Bad road exacerbating access
Odeyinka’s geographical location exacerbates the health centre’s challenges.
The community is situated at a considerable distance from the town. The absence of good roads and limited transportation options make it difficult to access the PHC.
The road from Ikire to Odeyinka is riddled with potholes filled with dirty water after every rainfall.

The journey from Ikire to Odeyinka takes up to an hour on a motorcycle. Mrs Ogundele told this reporter that she was always reluctant to refer her patients to the general hospital in the town because of the distance, scarcity of vehicles and the bad condition of the road.
Other PHCs
Many PHCs in Osun State are in similar conditions to the Odeyinka Health Centre. In the 12 that PREMIUM TIMES visited in six local government areas of the state – Ila-Orangun, Ilesha East, Irewole, Boluwaduro, Boripe and Aiyedire – two common things stood out: inadequate medical personnel and lack of equipment.
About a dozen officials of the PHCs who did not want their names mentioned because they were not authorised to speak, told this newspaper that they refer patients to the general hospitals or other hospitals due to their facilities’ lack of competence and facilities.
However, one common thing working in all PHCs visited was the solar-powered preservative fridge and equipment for immunisation.

Oke Ede PHC- Ila LGA
One of the popular health facilities in Ila Ward 3 is the Oke Ede PHC.
It was reconstructed and benefited from the 2019 PHC projects initiated by the immediate past governor of the state, Adeboyega Oyetola, currently Nigeria’s Minister of Marine and Blue Economy.
It was designed to have only one ward and one consulting room but no restroom. Although it had three beds, one was in disrepair.
The PHC has only three workers – a dental worker and two Community Health Extension Workers (CHEW), according to an official.
Over 10 communities rely on this PHC which lacks adequate power supply (no solar power), and no sufficient medical equipment.

Eripa – Boluwaduro LGA
The PHC in Eripa also lacked adequate staff despite admitting over 300 patients monthly and over 3,000 patients annually, according to an official document shown to this reporter.
Aside from the shortage of medical supplies, only nine persons were working in the health centre, including a laboratory scientist, a community health extension worker, one health assistant and one health attendant.

Iragbiji – Boripe LGA
The Iragbiji Police Medical Centre provides health services to residents of the community, including police personnel and their families.
While the Odeyinka PHC had one health worker, there were two health workers at the Iragbiji centre. One of them spoke with PREMIUM TIMES on the sorry state of the facility.
The worker said the PHC, which was reconstructed in 2022, lacked medical equipment and workers’ protective tools. The workers use their funds to buy equipment such as gloves, syringes, scissors and bandages to attend to patients.
She revealed that she is paid a monthly salary of N10,000 despite her qualifications, which she did not disclose to this newspaper.

Popo-Olupona – Aiyedire South LGA
There were seven health workers in Popo-Olupona PHC in Aiyedire South LGA. However, the centre did not have support staff such as cleaners, gardeners and security personnel.
Apart from this, its perimeter fence was collapsing while the two restroom doors had been damaged. Only one of the restrooms was in good use.

Ilesha- Ilesha East LGA
The story was equally pathetic in the popular Anaye PHC in Ilesha.
This reporter noticed that the centre had a broken ceiling while four of its six beds were damaged. Besides, the building had neither a gate nor security personnel manning it.
The health workers said that they lacked medical equipment despite the large areas it covers.
All these PHCs were visited by the reporter between October and November 2023.

Advent of PHCs in Nigeria
In 1978, Nigeria and other members of the World Health Organisation (WHO) adopted the Alma Ata Declaration which recognised that PHCs are a basic structure and functional unit of public health delivery systems. Since then many countries got grants to develop their PHCs.
In 2019, Governor Oyetola got a grant of $20.5 million to revamp and reconstruct the primary healthcare system of the state.
The fund was tagged, “Saving One Million Lives” and the then-governor awarded contracts to revamp and reconstruct 332 PHCs in the state.
Unfortunately, it was alleged that the contracts were awarded to party loyalists who did not deliver to the standards recommended for PHCs in Nigeria.
Minimum standard for PHC
According to the report of the Alma-Ata Conference on primary health care, PHC evolved from experiences with Basic Health Service (BHS) provision and delivery in several settings over the last couple of decades. However, it says PHC is a lot more than the provision of BHS.
WHO further identified four categories of indicators; namely, health policy, socio-economic factors, health service provision and quality of life indicators.
The Alma-Ata Conference also specified eight minimum health service areas that have since been referred to in many places as the minimum service components of PHC.
These are education on prevailing health problems and how to prevent them (health education); provision of water and basic sanitation (environmental health); adequate food supply and good nutrition (public health nutrition); maternal and child health including family planning (reproductive and family health), and immunisation against the common communicable diseases.
Others are control of common endemic diseases (epidemiology and disease control), treatment of common diseases and injuries (primary medical care), and provision of essential drugs (community pharmacy practice).
NPHCDA recommendation vs Osun PHCs
In Nigeria, the National Primary Health Care Development Agency (NPHCDA), established in 1992 following a recommendation by the World Health Organisation (WHO), is tasked with ensuring a proper and functional PHC system in the country. Its role includes stipulating infrastructural standards for PHC in Nigeria.
NPHCDA has a clear-cut specification and standard for establishing and constructing PHCs. According to the agency, a PHC should at first cover a minimum land area of 4,200 square metres and should have a detached building of at least 13 rooms, access to clean water possibly sourced from a motorised borehole, and functional separate male and female toilet facilities.
NPHCDA also noted that a PHC must be connected to the national grid and other regular alternative power sources, have a sanitary waste collection point and a waste disposal site, be clearly signposted – visible from both entry and exit points – be fenced and have a generator and gatehouses. Also, staff accommodation of 2 units of 1-bedroom flats should be provided within the premises.
The agency also recommends that a proper PHC structure comprises a building that has sufficient rooms and space to accommodate; Waiting/Reception areas for Child Welfare, ANC, Health Education and ORT corner, a staff station, 2 consulting rooms, an adolescent health service room, pharmacy and dispensing unit, two delivery rooms, maternity/lying-in section, in-patient ward section, laboratory, medical records area, injection/dressing area, minor procedures room, food demonstration area, kitchen store, among others.
According to the NPHCDA, an ideal PHC should have at least 24 workers on its staff, including a medical officer, four nurses or midwives, three Community Health Extension Workers, a pharmacy technician, an environmental officer, a medical record officer, a laboratory technician, two health attendants/assistants, two security personnel and one general maintenance staff, among others.
NPHCDA’s recommended equipment for PHCs includes consulting cubicle, artery forceps, bedpan, stainless steel, stainless bowls with stand, covered bowl for cotton wool, delivery couch, dissecting forceps, and dressing trolley, among others.
Sadly, all of the PHCs visited by this newspaper in Osun State fell short of these minimum standards.
However, these shortcomings are not peculiar to PHCs in Osun. Their abject conditions reflect the situation across Nigerian PHCs and hinder effective healthcare service delivery across the country.

Osun government speaks
The Osun State Commissioner for Health, Sola Akintola, said the state government led by Governor Ademola Adeleke has embarked on the renovation of the 332 PHCs that were not done well by his predecessor.
He said: “We want to renovate 332 PHCs, and I am happy to inform you that we have started with 50 and Odeyinka you mentioned is one of the 50 and it is at 60 per cent completion now. We are renovating and upgrading the PHCs, we want to dedicate it to be functioning 24 hours.
“At least there must be boreholes and electricity supply 24 hours. So we are giving solar to each of the 332 PHCs and functioning boreholes.”
Mr Akintola said the new administration noticed that apart from the fact that the PHCs have a shortage of personnel, there was also no provision for recruitment of staff for them in the budget inherited.
“So as regards that, the first thing we did was to have budgeting provision for that in the 2024 budget which has been approved. We will also be releasing the 40 per cent fund for the renovation. So before April runs out we are going to start the recruitment process. And we are releasing money for the second phase of the PHC,” the commissioner added.
Window dressing
The commissioner said what the previous administration did in the name of renovating the PHCs was just window dressing.
“You see there is a difference between actual renovation of PHCs and political renovation. You know we have to move around to see what they said they did and thank God the Odeyinka you went to is part of the one they claimed to have renovated.
“And what you met at Odeyinka is not different from the other 332 PHCs we are talking about. So what they did was just window dressing. So we want to renovate and upgrade now,” he said.
But contrary to the commissioner’s claim, when this reporter reached out to members of the community in April, they said the facility in Odeyinka was still in bad shape and there was no recent renovation, although some government officials visited the PHC at the end of February.
“No, nothing has been done here, maybe the model, but not at the PHC here. They only came around February ending and since then nothing has been done. In fact, we are currently cutting the grass around the facility and someone has been paid N4,500 to handle the thickly bushy areas within the premises,” a resident said.
This story was produced for the Frontline Investigative Programme and supported by the African Data Hub and Orodata Science.
Related Posts
State Government Accused of Extorting PHCs: Allegations and Impact Unveiled.
Jul 8, 2024
5 min read
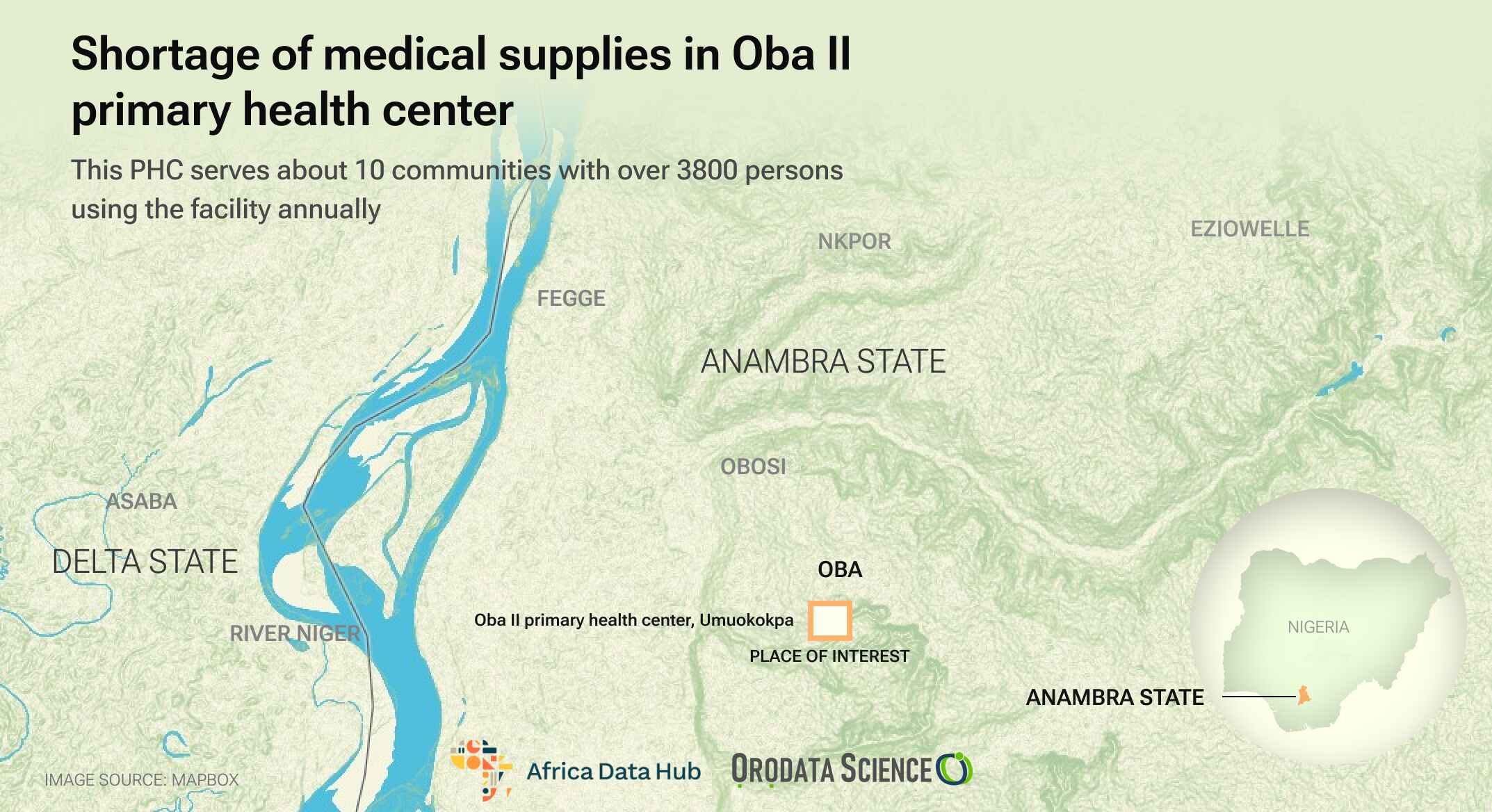
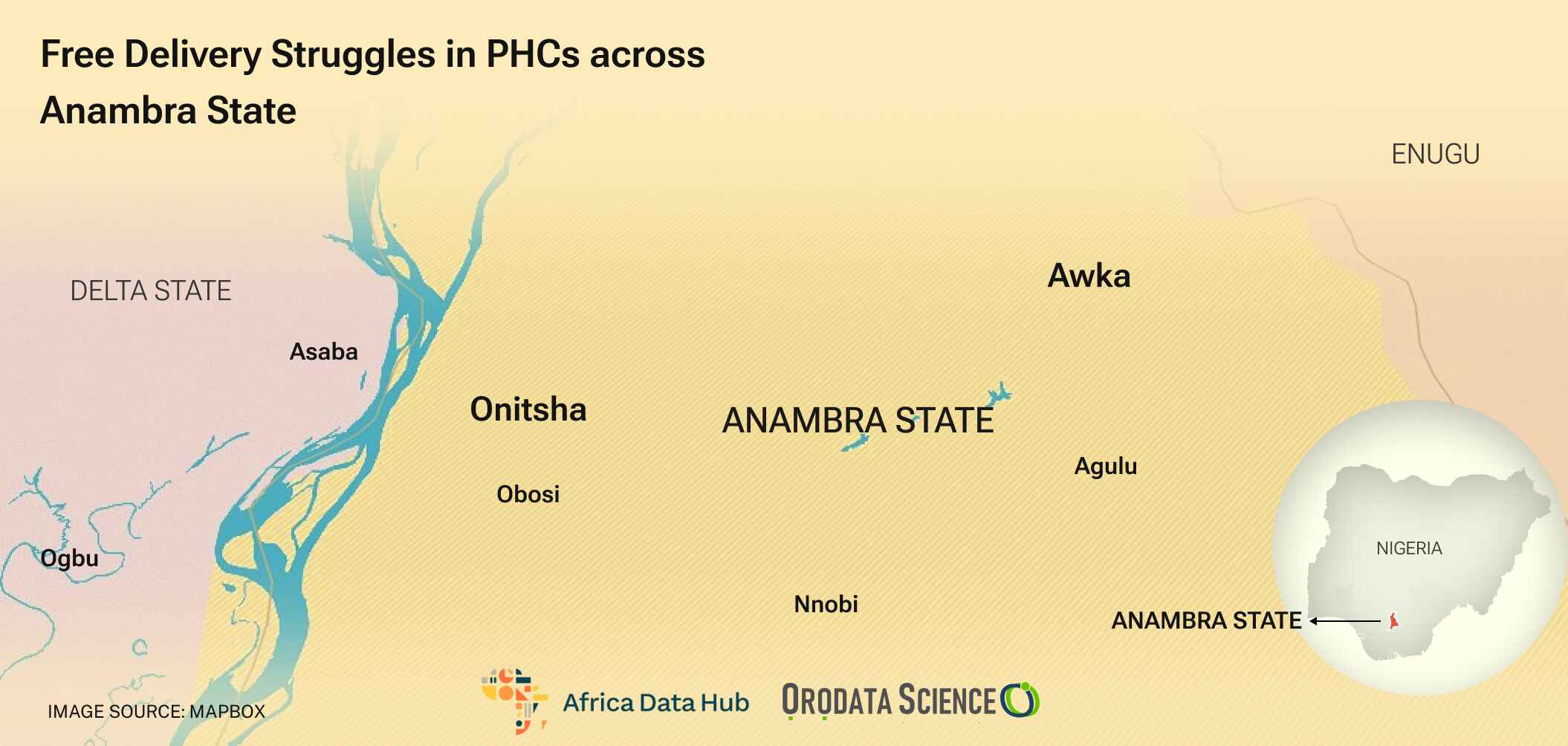
Overcoming Delivery Challenges: Free Services at Primary Health Centers in Anambra State
Jul 8, 2024
5 min read